Microbubbles to light the way to sentinel lymph nodes of breast cancer patients
By By Daniel Kane | 24 Feb 2011
Researchers at the University of California, San Diego are developing nonsurgical methods for identifying critical lymph nodes to help doctors determine courses of treatment for breast cancer patients. The ''sentinel lymph node'' is routinely biopsied or removed and dissected to determine the likelihood that the cancer has spread beyond the breast. Dr. Andrew Goodwin, a post doctoral fellow in the Department of Nanoengineering in the UC San Diego Jacobs School of Engineering recently received a Breast Cancer Postdoctoral Fellowship Award from the U.S. Department of Defense to use novel microbubbles to mark and interrogate the sentinel lymph node by means of a simple ultrasound scan.
 |
| Dr. Andrew Goodwin, a post doctoral fellow in the Department of Nanoengineering in the Jacobs School of Engineering recently received a Breast Cancer Postdoctoral Fellowship Award from the U.S. Department of Defense to use novel microbubbles to mark and interrogate the sentinel lymph node by means of a simple ultrasound scan. credit: UC San Diego |
''Since analysis of tumor stage is important for all breast cancer patients, this work would be expected to help many patients,'' explained Goodwin.
Cancer cells can detach from a primary tumor and enter the bloodstream by way of the lymph nodes. To determine if the cancer is spreading to other parts of the body, surgeons will biopsy or remove the lymph nodes to look for invading cells. Finding cancer cells in the lymph nodes often changes the course of treatment in an effort to kill any cancer cells that have already spread beyond the breast. Removing just the first, or sentinel, lymph node for analysis helps to reduce the likelihood of developing lymphedema, a painful, long-term swelling at the area of dissection.
The benefits of sentinel lymph node dissection for breast cancer patients were underscored by research findings recently published in The Journal of the American Medical Association.
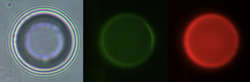 |
| Microscopy images of a polymer-dye-loaded microbubble. Left image: a bright field image of the microbubble showing the gas core. Center image: a green fluorescence image showing the dye-loaded polymer. Right image: a red fluorescence image showing the capture of free Rhodamine B, a fluorescent dye. credit: UC San Diego |
Ultrasound and Microbubbles
''I'm trying to develop a better way to mark the sentinel lymph node,'' says Goodwin. His approach involves using ultrasound – high-frequency sound waves used in medical imaging applications such as prenatal sonograms – and gas-filled microbubbles with fluorescent outer shells. These microbubbles capable of loading large amounts of dye are described in a recent article in the journal Soft Matter by Goodwin and coworkers.
If Goodwin's vision translates to the clinic, a physician would inject the fluorescent microbubbles into the tumor and then use ultrasound to visualize the bubbles as they drain away from the tumor and into the lymph nodes under the arm. Once the lymph nodes have been imaged and the sentinel lymph node identified, the radiologist will turn up the power of the ultrasound beam – but just in the area surrounding the sentinel lymph node. This will burst the microbubbles and release non-toxic fluorescent polymer that is designed to stick specifically in the lymph nodes for extended periods, allowing both the doctor and patient to adequately prepare for the lymph node dissection surgery.
For now, critical next steps include testing how the outer shell of the microbubbles interact with the lymph node lining, as well as tests in animal models.
Goodwin's UC San Diego collaborators include his mentor Sadik Esener, Director of the NanoTumor Center for Cancer Nanotechnology, and Professor of NanoEngineering and of Electrical and Computer Engineering at the Jacobs School of Engineering, and Radiology Professor Robert Mattrey, M.D. from the UCSD Moores Cancer Center. Last year, Dr. Goodwin also received a Pathway to Independence (K99) Award in Cancer Nanotechnology from the National Institute of Health on his work related to designing microbubbles for site-specific ultrasound imaging of malignant blood clots.



















